
Modern assisted human reproduction treatments have adapted to the needs and wishes of various different people and couples
Reciprocal in vitro fertilisation – also referred to as co-IVF or reception of oocytes from partner (ROPA) – is an assisted human reproduction treatment which enables homosexual female couples to both participate in pregnancy.
Motherhood is of course a commitment that goes beyond conception, carrying a pregnancy to term and ultimately giving birth, but many couples wish to actively participate in process of welcoming a baby into the world. Modern assisted human reproduction treatments include an in vitro fertilisation method available to homosexual women which involves both partners.
What is reciprocal in vitro fertilisation?
Reciprocal in vitro fertilisation (abbreviated to ROPA for the remainder of the succeeding elucidation) involves one partner providing an egg which is then fertilised in a laboratory, while their counterpart is the recipient via implantation in the uterus and then carries the pregnancy to full term.
Assisted human reproduction treatments are administered under strict control and upon the recommendation of specialists who will supervise proceedings from their inception.
ROPA begins with a complete gynaecological check-up and examination of both partners. Such analysis is essential as it determines who is best suited to donate and who better meets the demands of carrying a pregnancy to term. Although deciding who fulfils what role is one taken by the couple, objective medical data should be considered before reaching a conclusion.
Phases Of Reciprocal In Vitro Fertilisation (ROPA)
ROPA is based on the same methodology behind IVF treatments which involve sperm or egg donation, although the difference is one of the donors will be one of the future mothers.
Let us review steps previously outlined:
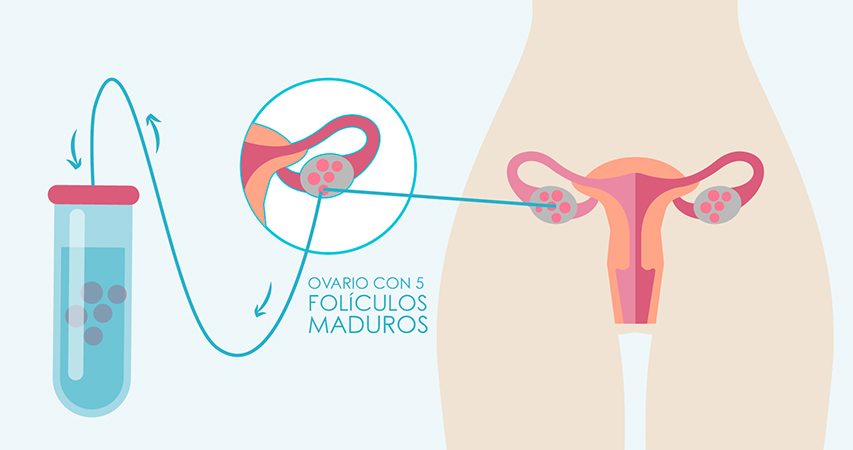
1. Ovarian stimulation of the woman who provides the eggs
The partner chosen as the egg donor will undergo ovarian stimulation treatment which involves a course of hormones taken over 10-12 days at home. Visitation to the clinic is only necessary for further analysis and ultrasound scans to assess the progression of ovulation.
2. Follicular Puncture
The extraction of developed eggs, known as follicular puncture, is a simple operation lasting around 15 minutes carried out under sedation. Follicles are checked beforehand to ensure they are the correct size before a dosage of hormone hCG is administered.
Around 36 hours after the final dosage, the puncture procedure is executed.
3. Embryo culture and preparation
Oocytes are fertilised in a laboratory using sperm provided by a sperm bank once criteria of standards and compatibility is met by the recipient couple.
The culture of embryos is meticulously monitored for a set period of time and are then classified according to their morphology and development to ensure the utmost quality.
The delay before implantation into the recipient’s uterus is two to six days.

4. Recipient preparation
The recipient undergoes a process prior to treatment which parallels that of the donor because menstrual cycles between the couple must be synchronised in order to ready the endometrium upon receiving an embryo at the time of implantation.
To ensure the layer or membrane covering the uterus has reached the required thickness between nine and 14 millimetres, an oestrogen and progesterone-based treatment is introduced while progression is monitored by ultrasound scans.
5. Embryo Transfer
Having prepared both the recipient and egg donor, the best embryo is then selected and introduced to the former of the couple so pregnancy can begin.
As with follicular puncture, transferring an embryo is a quick, painless and simple procedure which takes place in an operating theatre. Subsequent care is not required, unless medically advised depending on the circumstances of your specific case.
6. Post-Embryo Transfer Process
A pregnancy test can be taken after two weeks, while success rates of ROPA are high but are subject to factors such as age.
Regarded as a popuular fertility approach for homosexual female couples, the treatment allows for both women to be involved in pregnancy whether it be by donation or carrying the embryo to term.
Few people better understand what ROPA can signify to aspiring mothers than those who have undergone a treatment which permits those who previously thought they would be unable to contribute to a journey into parenthood to have an active participation.
